Altered States: Metabolic Disorders, Obesity and Disease
If you're an exercise professional, then you've probably had a client or two who had systemic inflammation, abdominal obesity, high blood pressure, and insulin resistance. Accordingly, you may have prescribed a regimen of hard work, clean eating and plenty of rest. Let’s hypothesize that your client was dedicated and did everything you asked. He pushed hard in the gym, ate like a monk and slept like a baby. But, in the end, his body failed to realize a significant aesthetic transformation and he eventually quit--leaving you scratching your head, wondering where you’d gone wrong.
The unfortunate reality of this example is that the effort was doomed from the start because you, the trainer, failed to properly assess, detect and address the client’s condition and, in doing so, you failed to recognize a unique but increasingly more prevalent medical condition called metabolic syndrome.
Syndrome X
So, what exactly is metabolic syndrome? Metabolic syndrome, also called syndrome X, is a pattern of metabolic risk factors that occur simultaneously; these include elevated blood pressure, abdominal adiposity, elevated plasma glucose, and systemic inflammation. It’s a progressive condition that is exacerbated by physical inactivity, advancing age, hormonal imbalance, and genetic predisposition. Metabolic syndrome is an energy sickness that disrupts the body’s autonomic ability and causes us to improperly produce and store energy.
It’s a particularly challenging clinical condition because of its complex molecular basis, which is still incompletely understood. However, impaired cellular metabolism has been suggested as an important factor in the chain of causation. This type of biochemical breakdown will often end in obesity, diabetes mellitus and heart disease.
Mitochondria dysfunction
Scientific investigation suggests that free radical based oxidative stress, which damages the mitochondria’s ability to function, may lead to metabolic syndrome. This begs the question, what role does healthy mitochondria play in the overall function of the human body?
A simplified explanation is that the mitochondria act as complex fuel processing plants that transform raw materials into energy. Primarily, the mitochondria convert the food we eat into Adenosine Triphosphate (ATP). This is done via the citric acid cycle (Krebs cycle) and the process of oxidative phosphorylation.
The production of ATP is the most important responsibility of the mitochondria. We use ATP for virtually everything we do, from eating, to picking up a newspaper, to long division. In fact your brain, heart and skeletal muscle have the highest number of mitochondria in the cytoplasm, which makes them more prone to the effects of mitochondrial dysfunction.
We know that cardiovascular disease and obesity are strongly related and diabetes is a known precursor to heart disease. Researchers who’ve observed patients with cardiovascular disease, noticed impaired oxidative phosphorylation and reduced mitochondrial content in their cells. This, coupled with an accumulation of adipose fat, often leads to a corruption of the body’s ability to properly burn excessive fat stores, leading to systemic inflammation and disease. The impaired function of the mitochondria, in this case, also can lead to an increase in the fatty lipids in your blood, perpetuating a cycle of fat storage and metabolic dysfunction.
The Homeostatic Process
A growing body of evidence has demonstrated a link between various disturbances in mitochondrial function and type 2 diabetes. The pathophysiology of type 2 diabetes mellitus (DM) is varied and complex. However, the association of diabetes with obesity and inactivity indicates an important, and potentially pathogenic, link between fuel and energy homeostasis and the emergence of metabolic disease. Given the central role for mitochondria in fuel utilization and energy production, disordered mitochondrial function at the cellular level may impact whole-body metabolic homeostasis. Thus, I offer the hypothesis that defective mitochondria can lead an apparently healthy person down the road to disease.
New research supports these assertions and suggests that flawed mitochondrial function may lead to a premature aging phenomenon by negatively impacting heart, brain, and skeletal muscle. This phenomenon may cause relatively young individuals to encounter disease prematurely. It’s a sad reality that, in the past, these diseases where normally only associated with the elderly. This is an important concept to share with your client base; the idea that mitochondria dysfunction causes “premature aging” and the onset of disease is a salient and startling concept and may act as a catalyst in the client’s recognition and acceptance of the aesthetic limitations they may encounter when training.
So, why am I still fat?
Over the past two decades, we’ve seen a worldwide increase in societal obesity and disease that may be attributed to Syndrome X. Modern scientists and fitness gurus alike have offered vast theoretical solutions to this pandemic. Unfortunately, concepts like calories in calories out, Zumba and the food pyramid have come up woefully short, leaving most of us feeling sick and empty. This failure can be attributed to industry wide intellectual inbreeding, societal changes, governmental shortsightedness and, most importantly, the insular nature of two symbiotic fields, exercise science and medicine.
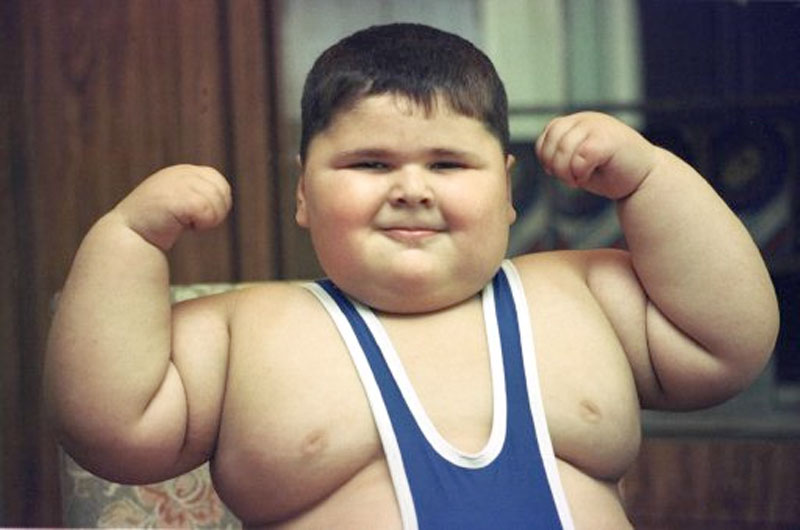
Since metabolic syndrome causes the afflicted to experience symptoms synonymous with premature aging disorders and its associated diseases, it would certainly be advisable to seek a solution in conjunction with experts who regularly deal with geriatrics. Yet the free exchange of ideas between the exercise scientist and the medical doctor is sporadic at best. This is unfortunate because the co-mingling of ideas between these two fields could lead to innovative treatment options for a broad spectrum of pathologies, especially the geriatric patient who experiences syndrome X-like symptoms but is unable to exercise due to impaired hormone production, frailty, immobility and compromised neurophysiology. Fortunately, there’s hope for the young client with metabolic syndrome. I believe they’re primed to thrive in an exercise based therapy environment, which, in turn, may aid in stemming the current state of childhood obesity in our country.
Huckster Inc.
The client with metabolic syndrome will likely enter a fitness program looking to lose weight. This isn’t always easy to accomplish due to their unique pathology. To make matters worse, the experts-by-proxy and media types have created unrealistic body-image expectations. Some of these same hucksters espouse “one-size fits all” training and embrace methods like muscle confusion, metcon bombs and the occasional “big Jim” as viable solutions for every client that walks through their door.
These factors have contributed to an increasingly misinformed public who’s grown to expect results that mimic those seen on The Biggest Loser. This is a big hurdle to overcome as a trainer and a business owner; misinformation has made our job increasingly difficult, especially when proposing honest expectations for trainees affected by an energy-sickness.
However, I think it’s important to openly discuss what the syndrome X client should realistically expect when training. The reality is that the bulk of their initial change will likely occur biologically, which isn’t an easy concept to sell. So, you’ll have to help them re-prioritize their expectations by placing a smaller emphasis on aesthetic change while increasing the focusing on disease prevention, strength and mobility.
In addition to establishing these new expectations, we should encourage the client to monitor their progress through a health care provider, by using blood profiles as a pre and post-training metric. Although these initial efforts may be time consuming, they will likely pay dividends in the form of increased client retention and goodwill.
Homeostatic Training
The prescription of diet and exercise is far too general for the complex set of variables encountered when dealing with a client who has metabolic syndrome. This is where a talented team comprised of trainer and physician can offer help in the form of direction, education and intervention. The educational component is the most important aspect of this recipe and it’s imperative that the client receive a full medical screening prior to training in order to establish baselines and/or training restrictions.
Next, you’ll need to get the client to accept that their unique condition will conspire to thwart many of their efforts in the gym. The aesthetic result that many people experience through training may elude this individual, since they’re patently different biologically. This client may never “look good naked,” but they can certainly become healthier. This proposition may not be easy for the client to accept, until they have a sound understanding of their condition. This can be achieved by sharing the rudimentary concept that training and diet are simply forms of stimulus used to manipulate the homeostatic process. This is “super compensation theory” in a nutshell: apply an appropriate stimulus to the body and get a positive response in return. Unfortunately, when a client has a homeostatic process that is damaged or corrupt, it makes it increasingly difficult to illicit change, particularly of an aesthetic nature.
This may seem like a less than optimistic outlook but it’s a realistic one and it shouldn't be glossed over in an attempt to appease. Our job, as professionals, is to educate the client and assist them in understanding how their body may change via exercise and diet. We currently know that aerobic interval training, dietary supplementation of fish oil, carbohydrate restriction and resistance training, are the best non-medical approaches in treating metabolic dysfunction.
Clearly, I’ve distilled these therapeutic solutions for the sake of content and time. However, I also recognize that they deserve a more in-depth descriptive narrative. With this in mind, I intend to continue my research through my clients and their training in order to build a larger body of evidence to support my theory. This body of work will focus on the psychological, physiological, biological and sociological changes that these clients experience through their efforts.
Since medical research is advancing at an astonishing rate and will continue to provide us with new data on the nature of this syndrome, it becomes increasingly important for the exercise professional to remain vigilant in disseminating the latest scientific research. With this said, it’s my belief that the combined efforts of the medical doctor and the trainer will likely lead to a solution to this complicated problem. Industry wide sharing of ideas, methods and data, offers us the best opportunity to develop new, evidence based therapies for society at large. These therapies may have far reaching ramifications and could eventually be used to treat and train a broad spectrum of clients, both healthy and sick.
Paresh Dandona, Ahmad Aljada, Ajay Chaudhuri, Priya Mohanty, and Rajesh Garg
Metabolic Syndrome: A Comprehensive Perspective Based on Interactions Between Obesity, Diabetes, and Inflammation. (Circulation. 2005;111:1448-1454.) 2005 American Heart Association, Inc.
2 Garth L. Nicolson. Metabolic Syndrome and Mitochondrial Function: Molecular Replacement and Antioxidant Supplements to Prevent Membrane Peroxidation and Restore Mitochondrial Function Journal of Cellular Biochemistry 9999:1–18 (2007)
3Mary-Elizabeth Patti and Silvia Corvera. The Role of Mitochondria in the Pathogenesis of Type 2 Diabetes, Endocrine Reviews June 1, 2010 vol. 31 no. 3 364-395
4 Douglas C. Wallace. A Mitochondrial Paradigm of Metabolic and Degenerative Diseases, Aging, and Cancer: A Dawn for Evolutionary Medicine. Annual Review of Genetics Vol. 39: 359-407 (Volume publication date December 2005)
5 Aguilera AA, Díaz GH, Barcelata ML, Guerrero OA, Ros RM. Effects of fish oil on hypertension, plasma lipids, and tumor necrosis factor-alpha in rats with sucrose-induced metabolic syndrome. J Nutr Biochem. 2004 Jun; 15(6):350-7.
6 Jan Sundell. Resistance Training Is an Effective Tool against Metabolic and Frailty Syndromes. Advances in Preventive Medicine, Volume 2011 (2011), Article ID 984683, 7 pages
doi:10.4061/2011/984683
7 Arnt Erik Tjønna, MSc; Sang Jun Lee, PhD; Øivind Rognmo, MSc; Tomas O. Stølen, MSc; Anja Bye, MSc; Per Magnus Haram, PhD; Jan Pål Loennechen, PhD; Qusai Y. Al-Share, MSc; Eirik Skogvoll, PhD; Stig A. Slørdahl, PhD; Ole J. Kemi, PhD; Sonia M. Najjar, PhD*; Ulrik Wisløff, PhD. Aerobic Interval Training Versus Continuous Moderate Exercise as a Treatment for the Metabolic Syndrome, (Circulation. 2008;118:346-354.) © 2008 American Heart Association, Inc.
8 Jeff S Volek1 and Richard D Feinman. Carbohydrate restriction improves the features of Metabolic Syndrome. Published: 16 November 2005 Nutrition & Metabolism 2005, 2:31 doi:10.1186/1743-7075-2-31
The unfortunate reality of this example is that the effort was doomed from the start because you, the trainer, failed to properly assess, detect and address the client’s condition and, in doing so, you failed to recognize a unique but increasingly more prevalent medical condition called metabolic syndrome.
Syndrome X
So, what exactly is metabolic syndrome? Metabolic syndrome, also called syndrome X, is a pattern of metabolic risk factors that occur simultaneously; these include elevated blood pressure, abdominal adiposity, elevated plasma glucose, and systemic inflammation. It’s a progressive condition that is exacerbated by physical inactivity, advancing age, hormonal imbalance, and genetic predisposition. Metabolic syndrome is an energy sickness that disrupts the body’s autonomic ability and causes us to improperly produce and store energy.
It’s a particularly challenging clinical condition because of its complex molecular basis, which is still incompletely understood. However, impaired cellular metabolism has been suggested as an important factor in the chain of causation. This type of biochemical breakdown will often end in obesity, diabetes mellitus and heart disease.
Mitochondria dysfunction
Scientific investigation suggests that free radical based oxidative stress, which damages the mitochondria’s ability to function, may lead to metabolic syndrome. This begs the question, what role does healthy mitochondria play in the overall function of the human body?
A simplified explanation is that the mitochondria act as complex fuel processing plants that transform raw materials into energy. Primarily, the mitochondria convert the food we eat into Adenosine Triphosphate (ATP). This is done via the citric acid cycle (Krebs cycle) and the process of oxidative phosphorylation.
The production of ATP is the most important responsibility of the mitochondria. We use ATP for virtually everything we do, from eating, to picking up a newspaper, to long division. In fact your brain, heart and skeletal muscle have the highest number of mitochondria in the cytoplasm, which makes them more prone to the effects of mitochondrial dysfunction.
We know that cardiovascular disease and obesity are strongly related and diabetes is a known precursor to heart disease. Researchers who’ve observed patients with cardiovascular disease, noticed impaired oxidative phosphorylation and reduced mitochondrial content in their cells. This, coupled with an accumulation of adipose fat, often leads to a corruption of the body’s ability to properly burn excessive fat stores, leading to systemic inflammation and disease. The impaired function of the mitochondria, in this case, also can lead to an increase in the fatty lipids in your blood, perpetuating a cycle of fat storage and metabolic dysfunction.
The Homeostatic Process
A growing body of evidence has demonstrated a link between various disturbances in mitochondrial function and type 2 diabetes. The pathophysiology of type 2 diabetes mellitus (DM) is varied and complex. However, the association of diabetes with obesity and inactivity indicates an important, and potentially pathogenic, link between fuel and energy homeostasis and the emergence of metabolic disease. Given the central role for mitochondria in fuel utilization and energy production, disordered mitochondrial function at the cellular level may impact whole-body metabolic homeostasis. Thus, I offer the hypothesis that defective mitochondria can lead an apparently healthy person down the road to disease.
New research supports these assertions and suggests that flawed mitochondrial function may lead to a premature aging phenomenon by negatively impacting heart, brain, and skeletal muscle. This phenomenon may cause relatively young individuals to encounter disease prematurely. It’s a sad reality that, in the past, these diseases where normally only associated with the elderly. This is an important concept to share with your client base; the idea that mitochondria dysfunction causes “premature aging” and the onset of disease is a salient and startling concept and may act as a catalyst in the client’s recognition and acceptance of the aesthetic limitations they may encounter when training.
So, why am I still fat?
Over the past two decades, we’ve seen a worldwide increase in societal obesity and disease that may be attributed to Syndrome X. Modern scientists and fitness gurus alike have offered vast theoretical solutions to this pandemic. Unfortunately, concepts like calories in calories out, Zumba and the food pyramid have come up woefully short, leaving most of us feeling sick and empty. This failure can be attributed to industry wide intellectual inbreeding, societal changes, governmental shortsightedness and, most importantly, the insular nature of two symbiotic fields, exercise science and medicine.
Since metabolic syndrome causes the afflicted to experience symptoms synonymous with premature aging disorders and its associated diseases, it would certainly be advisable to seek a solution in conjunction with experts who regularly deal with geriatrics. Yet the free exchange of ideas between the exercise scientist and the medical doctor is sporadic at best. This is unfortunate because the co-mingling of ideas between these two fields could lead to innovative treatment options for a broad spectrum of pathologies, especially the geriatric patient who experiences syndrome X-like symptoms but is unable to exercise due to impaired hormone production, frailty, immobility and compromised neurophysiology. Fortunately, there’s hope for the young client with metabolic syndrome. I believe they’re primed to thrive in an exercise based therapy environment, which, in turn, may aid in stemming the current state of childhood obesity in our country.
Huckster Inc.
The client with metabolic syndrome will likely enter a fitness program looking to lose weight. This isn’t always easy to accomplish due to their unique pathology. To make matters worse, the experts-by-proxy and media types have created unrealistic body-image expectations. Some of these same hucksters espouse “one-size fits all” training and embrace methods like muscle confusion, metcon bombs and the occasional “big Jim” as viable solutions for every client that walks through their door.
These factors have contributed to an increasingly misinformed public who’s grown to expect results that mimic those seen on The Biggest Loser. This is a big hurdle to overcome as a trainer and a business owner; misinformation has made our job increasingly difficult, especially when proposing honest expectations for trainees affected by an energy-sickness.
However, I think it’s important to openly discuss what the syndrome X client should realistically expect when training. The reality is that the bulk of their initial change will likely occur biologically, which isn’t an easy concept to sell. So, you’ll have to help them re-prioritize their expectations by placing a smaller emphasis on aesthetic change while increasing the focusing on disease prevention, strength and mobility.
In addition to establishing these new expectations, we should encourage the client to monitor their progress through a health care provider, by using blood profiles as a pre and post-training metric. Although these initial efforts may be time consuming, they will likely pay dividends in the form of increased client retention and goodwill.
Homeostatic Training
The prescription of diet and exercise is far too general for the complex set of variables encountered when dealing with a client who has metabolic syndrome. This is where a talented team comprised of trainer and physician can offer help in the form of direction, education and intervention. The educational component is the most important aspect of this recipe and it’s imperative that the client receive a full medical screening prior to training in order to establish baselines and/or training restrictions.
Next, you’ll need to get the client to accept that their unique condition will conspire to thwart many of their efforts in the gym. The aesthetic result that many people experience through training may elude this individual, since they’re patently different biologically. This client may never “look good naked,” but they can certainly become healthier. This proposition may not be easy for the client to accept, until they have a sound understanding of their condition. This can be achieved by sharing the rudimentary concept that training and diet are simply forms of stimulus used to manipulate the homeostatic process. This is “super compensation theory” in a nutshell: apply an appropriate stimulus to the body and get a positive response in return. Unfortunately, when a client has a homeostatic process that is damaged or corrupt, it makes it increasingly difficult to illicit change, particularly of an aesthetic nature.
This may seem like a less than optimistic outlook but it’s a realistic one and it shouldn't be glossed over in an attempt to appease. Our job, as professionals, is to educate the client and assist them in understanding how their body may change via exercise and diet. We currently know that aerobic interval training, dietary supplementation of fish oil, carbohydrate restriction and resistance training, are the best non-medical approaches in treating metabolic dysfunction.
Clearly, I’ve distilled these therapeutic solutions for the sake of content and time. However, I also recognize that they deserve a more in-depth descriptive narrative. With this in mind, I intend to continue my research through my clients and their training in order to build a larger body of evidence to support my theory. This body of work will focus on the psychological, physiological, biological and sociological changes that these clients experience through their efforts.
Since medical research is advancing at an astonishing rate and will continue to provide us with new data on the nature of this syndrome, it becomes increasingly important for the exercise professional to remain vigilant in disseminating the latest scientific research. With this said, it’s my belief that the combined efforts of the medical doctor and the trainer will likely lead to a solution to this complicated problem. Industry wide sharing of ideas, methods and data, offers us the best opportunity to develop new, evidence based therapies for society at large. These therapies may have far reaching ramifications and could eventually be used to treat and train a broad spectrum of clients, both healthy and sick.
Paresh Dandona, Ahmad Aljada, Ajay Chaudhuri, Priya Mohanty, and Rajesh Garg
Metabolic Syndrome: A Comprehensive Perspective Based on Interactions Between Obesity, Diabetes, and Inflammation. (Circulation. 2005;111:1448-1454.) 2005 American Heart Association, Inc.
2 Garth L. Nicolson. Metabolic Syndrome and Mitochondrial Function: Molecular Replacement and Antioxidant Supplements to Prevent Membrane Peroxidation and Restore Mitochondrial Function Journal of Cellular Biochemistry 9999:1–18 (2007)
3Mary-Elizabeth Patti and Silvia Corvera. The Role of Mitochondria in the Pathogenesis of Type 2 Diabetes, Endocrine Reviews June 1, 2010 vol. 31 no. 3 364-395
4 Douglas C. Wallace. A Mitochondrial Paradigm of Metabolic and Degenerative Diseases, Aging, and Cancer: A Dawn for Evolutionary Medicine. Annual Review of Genetics Vol. 39: 359-407 (Volume publication date December 2005)
5 Aguilera AA, Díaz GH, Barcelata ML, Guerrero OA, Ros RM. Effects of fish oil on hypertension, plasma lipids, and tumor necrosis factor-alpha in rats with sucrose-induced metabolic syndrome. J Nutr Biochem. 2004 Jun; 15(6):350-7.
6 Jan Sundell. Resistance Training Is an Effective Tool against Metabolic and Frailty Syndromes. Advances in Preventive Medicine, Volume 2011 (2011), Article ID 984683, 7 pages
doi:10.4061/2011/984683
7 Arnt Erik Tjønna, MSc; Sang Jun Lee, PhD; Øivind Rognmo, MSc; Tomas O. Stølen, MSc; Anja Bye, MSc; Per Magnus Haram, PhD; Jan Pål Loennechen, PhD; Qusai Y. Al-Share, MSc; Eirik Skogvoll, PhD; Stig A. Slørdahl, PhD; Ole J. Kemi, PhD; Sonia M. Najjar, PhD*; Ulrik Wisløff, PhD. Aerobic Interval Training Versus Continuous Moderate Exercise as a Treatment for the Metabolic Syndrome, (Circulation. 2008;118:346-354.) © 2008 American Heart Association, Inc.
8 Jeff S Volek1 and Richard D Feinman. Carbohydrate restriction improves the features of Metabolic Syndrome. Published: 16 November 2005 Nutrition & Metabolism 2005, 2:31 doi:10.1186/1743-7075-2-31
|
Eric Auciello is a passionate advocate for personal fitness. Part personal trainer, part philosopher, and part drill-sergeant, he owns and operates Phase Five Inc. a private strength and conditioning facility located in Brandon, Florida. |
Search Articles
Article Categories
Sort by Author
Sort by Issue & Date
Article Categories
Sort by Author
Sort by Issue & Date